 The biggest ever transformation of community mental health services is underway across Greater Manchester.
The biggest ever transformation of community mental health services is underway across Greater Manchester.
We want to work with patients, carers, family members and partners to get things right.
If you have any questions, or want to know where your borough is up to, or get involved, details are provided below.
What is community mental health transformation?
The transformation is part of the national NHS long term plan (opens in new window), which sets out a commitment to making sure everyone can get the mental health support they need (opens in new window).
The aim is to improve mental health care and support for adults and older adults.
Lots of services and professionals are working together, including our mental health staff, primary care (GPs), social care, colleagues from voluntary community and social enterprise (VCSE) services, people with lived experience, carers, and others.
We’re working towards making services more joined up, easier to access and more consistent. This will help make sure patients, carers and families get the right care and support in the right place, as early as possible.
Each borough is developing a new way of working together (known as living well) based on the needs of local people.
What do the changes look like?
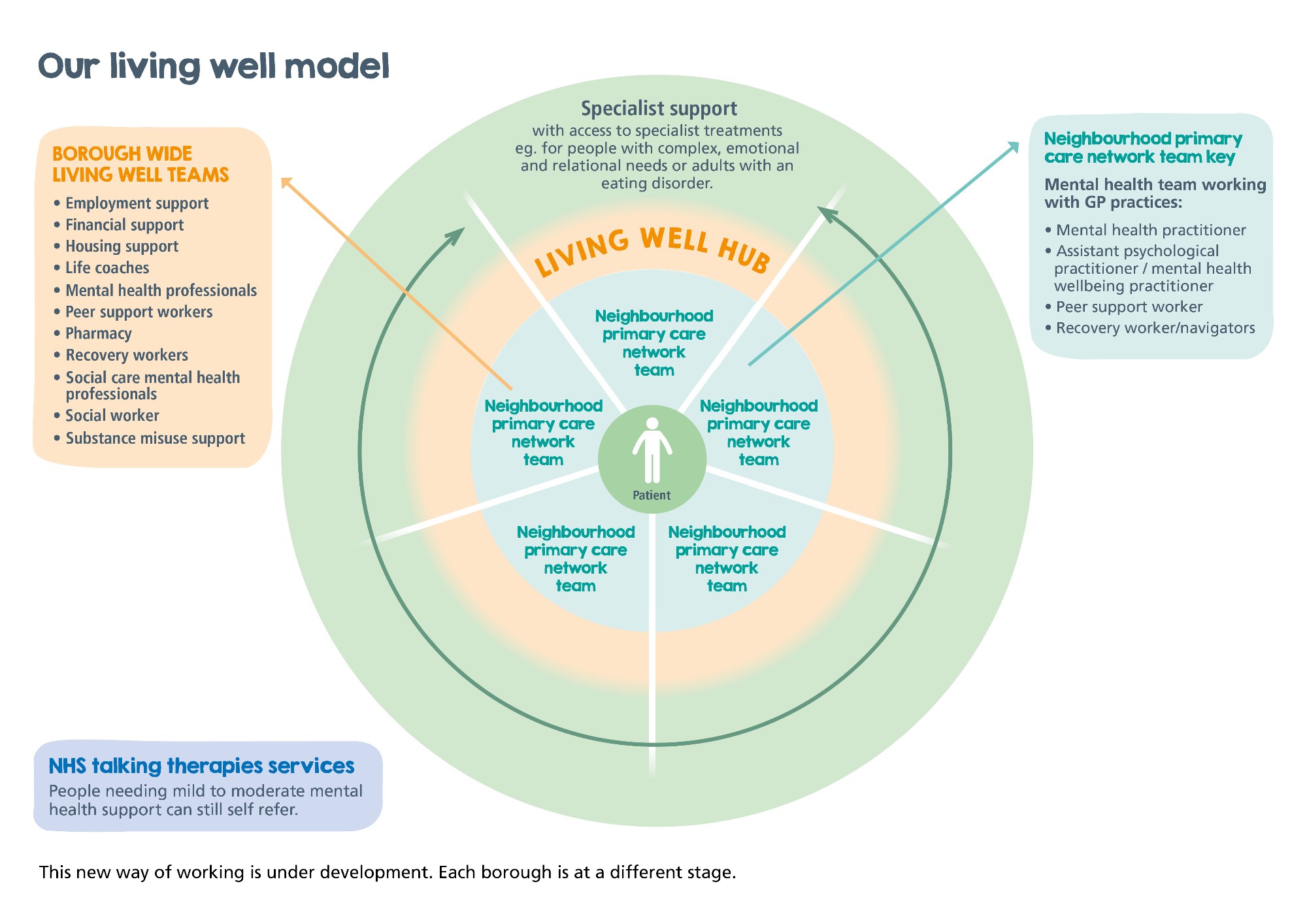
There’s a huge amount of work happening to transform community mental health services. Here's a summary of our new way of working. The diagram below shows how everything will fit together.
Improved joint working - primary care networks and living well teams
- Groups of GP practices are working with mental and physical health services, social care, pharmacy, hospital and voluntary services. These groups are known as primary care networks (opens in new window)
- Lots of new mental health staff have been recruited to work with many of the primary care networks. This includes mental health practitioners (opens in new window), psychological practitioners / mental health wellbeing practitioners (opens in new window), peer support workers, and recovery workers
- These professionals work in several GP practices to provide you with mental health support
- Working with your GP, they'll look at what support you need and if they can meet all your needs.
- If you need more or different support than they can offer, they'll have a discussion with other professionals to agree who is best to help you. This could include a pharmacist, social worker, employment, financial or housing support, voluntary, community and social enterprise (VCSE) colleagues, drug and alcohol, domestic abuse or loneliness support or another specialist.
- These professionals meet regularly - together they're known as the living well team.
- You might receive support from one professional, or several at the same time.
- Some people with complex needs may need more support than the living well team can offer. They’ll be linked in with their local community health team, which are currently making improvements to how they support people (details below). Depending on their needs, they may benefit from one of our of our new specialist services or treatments.
New specialist services and treatments
As part of the transformation, we’ve developed some new specialist services including:
- Treatments for people with complex emotional and relational needs, which means they experience significant difficulties in regulating their emotions or with interpersonal relationships. Read more about complex emotional and relational needs treatments (opens in new window).
- A community rehabilitation team to support people to be safely discharged from our rehab and high support units and bring home people who are placed in a unit outside the area. Read more about the community rehabilitation team (opens in new window).
- We've also worked with our partner Greater Manchester Mental Health to develop a specialist community-based service for adults with an eating disorder. Read more about the eating-disorders service (opens in new window).
Improved care planning and recovery progress measurement
Care planning:
Our community mental health teams provide assessment, treatment, and care to people with severe and long-term mental health problems.
Currently they use a care programme approach, which involves a care co-ordinator being responsible for planning and overseeing the care of several patients at one time. A review is usually done every six or twelve months.
There are lots of benefits to the care programme approach, which we want to keep. But we know we need a fresh approach to ensure care is higher quality, more flexible and better meets your needs.
We’re working with our patients, carers, families, staff, and partners locally and nationally to make improvements. The new approach will include the following principles:
- Moving away from clinician-led generic care co-ordination to an approach where you and your care team jointly agree actions and goals that are important to you.
- You’ll continue to have a key worker to ensure consistency and clarity – but many different professionals will provide your care. Depending on your needs, this could include a nurse, social worker, occupational therapist, employment/vocational support, housing, substance misuse. All professionals involved will share responsibility for your care.
- Your care plan will be reviewed when it’s needed, rather than at a set point in time. And we want you to feel confident to request reviews and changes whenever you want. We’ll also support you to be familiar and understand your care plan, so you can feel more in control, independent and empowered.
- We’ll better support and involve carers, including improving our communication with you, proactively involving you in your loved one’s care plan and making sure you receive more support focused on your own needs.
Measuring recovery progress:
Linked to improved care planning, we’re also developing new ways to measure your recovery, known as patient reported outcome measures (PROMs).
These are questionnaires that ask about your symptoms, wellbeing, and quality of life. It helps your clinician find out what goals you want to achieve from your support, care, and treatment.
Your goals could include having reduced or no symptoms, volunteering in the community, returning to a job you love, taking up a new or past hobby, seeing more of your family and friends, or something else that helps you lead a more fulfilling life.
Your clinician will ask you to complete some questionnaires at the start of your care, throughout, and at the end.
Your responses will provide your care team with a score or rating that they can use to see if you're getting better, staying the same, or getting worse. Your care team may also use other ways to monitor your progress and experiences, depending on what’s right for your needs.
The new patient reported outcome measures will be used by all community-based mental health services and professionals, including the practitioners who work in GP practices, living well teams, community mental health teams and our new specialist services.
If you have any questions about these planned improvements to your care, please speak to your clinician or care team.
What are the benefits?
The aim is that you will benefit from improved recovery progress and quality of life by:
- Easily and quickly getting the right care for your needs.
- Easily being able to get more or less help, to meet your changing needs.
- Having your all-round needs met in a joined-up way, including mental and emotional health, physical health, and social issues (e.g. substance addiction, isolation, housing, finances, employment etc).
- Being supported to focus on your strengths and improve your self-management skills
- Having to “repeat your story” less times
- Receiving greater support from your families, carers, and social networks, and opportunities to participate in their local community.
- Receiving more peer support from people with lived experience of mental health issues, who can connect and understand using their own experiences.
- Being supported to feel more independent, confident, and empowered.
- Having an all-round better experience of using services.
Patient case studies
- Christine - Rochdale (to be added)
- Sufyan - Bury
- Fatima - Rochdale
- Michael - Rochdale
When will the transformation be complete?
Transforming services is very complex and it’ll take time to get things right.
We’ve made lots of progress already, but we know there's more to do.
We’ll need to continually review and improve services based on learning and feedback from our patients, carers, family members, and other key people.
And we're learning from what has worked in other areas. Our leads visited colleagues in Lambeth, London. This is where the "living well programme" was first established over 10 years ago. Read more about their visit to Lambeth (opens in new window).
Progress in your borough
Click on the link below for an update on progress in your borough.
We'll keep this page updated and share key updates on Twitter, Facebook, LinkedIn, and Instagram. Follow us @PennineCareNHS.
- Bury (opens in new window)
- Heywood, Middleton or Rochdale (opens in new window)
- Oldham (opens in new window)
- Stockport (opens in new window)
- Tameside or Glossop (opens in new window)
If you live in one of the other Greater Manchester boroughs, visit the Greater Manchester Mental Health NHS Foundation Trust website.
Get involved and find out more
We’re already involving lots of people with lived experience, families, carers and others in the transformation work, but we always welcome input and feedback from people in our communities.
If you’d like to help us get things right, click here for details of how to get involved.
Key publications
- The Community Mental Health Framework for Adults and Older Adults (opens in new window)
- Living well in Greater Manchester (opens in new window)
- Patient Reported Outcome Measures (PROMs) for People with Severe Mental Illness in Community Mental Health Settings (opens in new window)